KEY POINTS
- Suicide is a leading cause of death in the United States.
- Knowing how to intervene when someone shows warning signs of suicidal thoughts and impulses is critical.
- Don't be afraid to be direct about your concern; assess their lethality and then intervene with a plan of action.

I think it is important to share this suicide intervention plan for a number of reasons: (1) the news about two high-profile athletes who died by suicide, Katie Meyer and Sarah Shulze, (2) a recent national pollthat found only one in four parents (25 percent) think their adolescent would definitely talk with them about a mental health issue, (3) the reality that we know overindulged adolescents and emerging adults engage in higher frequencies of dysfunctional thinking, which leads to depression, (4) according to the CDC, suicide is a leading cause of death in the United States with 45,979 deaths in 2020, and (5) you can do something about it if you know what to do.
Source: khoa võ/Pexels
A true story
I was petrified, absolutely scared to death! It was a little after 3 a.m. when I hung up the phone. Jackie* [name has been changed] had just called to tell me she was going to commit suicide. She said, “I have the pills in my hand, and I’m ready to take them, but I just don’t know….”
Immediately, I was awake from a jolt of adrenaline. “No, Jackie, don’t do it! Just wait till I get there before you do anything. Promise me.”
I was a psychology major at the University of Oklahoma, and I didn’t have the foggiest idea of what to do next.
We spent the rest of the night at Perkins, drinking coffee and talking until I came up with a plan. I figured, “As long as she’s here with me, she won’t kill herself.” Finally, after spending the longest five hours of my life, it was eight o’clock. I took her to my campus pastor’s home. Surely he’d had some experience with suicide and would know what to do. And he did!
This event happened almost 50 years ago, but I haven’t forgotten that queasy, anxious, helpless feeling in the pit of my stomach caused by not knowing what to do. Since then, I have encountered many “Jackies” contemplating suicide. I would like to share what I have learned so that if the need arises, you, too, will know what to do. (Click here to download the Suicide Intervention Plan below.)
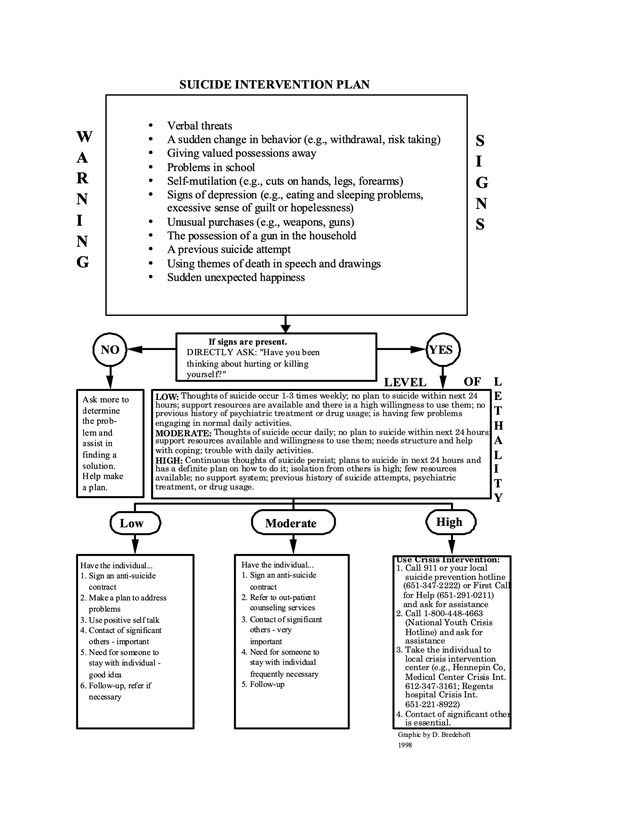
Source: David J Bredehoft, Ph.D.
Be observant.
Look and listen. Most individuals contemplating suicide let the people around them know indirectly through their behavior (see warning signs of suicidal behavior). They may say things like, “You’ll really miss me when I’m gone,” or, “It doesn’t really matter anymore.” They suffer from depression, have trouble sleeping and eating, have problems at work or school, or suddenly give away prized possessions as if they are executing their last will and testament.
Don’t be afraid to ask.
If you are picking up signals that something is wrong, ask. Don’t beat around the bush or hint at it; simply be upfront about it. Ask directly by saying, “Have you been thinking about hurting, harming, or killing yourself?” Don’t worry: You will not push them over the edge. The most common reaction from a suicidal person when asked is a feeling of relief (“Finally, someone sees my distress!”).
If the answer is no, find out more about the problem and encourage problem-solving. Assist in making a plan and suggest they take advantage of resources of which they may not be aware. If the answer is yes, your next task is to assess the individual’s lethality.
Assess their lethality.
Show your concern. Be genuine. In doing so, you will develop rapport and trust. In a non-judgmental way, ask questions that yield vital information. “How often have you been having these thoughts? “Do you have a concrete plan to carry it out?” “If so, what is your plan?” “Have you taken any steps toward the plan?” Finally, determine how lethal the individual is (see levels of lethality in the Suicide Intervention Plan).
THE BASICS
Intervene with a plan of action.
Follow the guidelines suggested for each level of lethality: low, moderate, or high. If the individual is low or moderate in lethality, have them sign an Anti-Suicide Contract (here is an example). Fortunately, most individuals will follow this contract. If the individual is high in lethality, dial 988 the National Suicide Prevention Lifeline, and ask for assistance. Or, if the person is willing, take them to a local hospital crisis center. A local hospital crisis center will be able to assess the situation and even hospitalize if necessary.
In addition, anytime the Suicide Intervention Plan suggests “make a plan,” it is referring to Glasser’s eight components for a plan (1989):
- Simple
- Small
- Something to do, not stop doing
- Dependent on what you do, not what others do
- Specific (what, when, how)
- Repetitive
- Immediate
- One to which you can make a commitment.
A happy ending for Jackie:
A few years following this incident, I ran into Jackie at Denver International Airport. She is a flight attendant for Delta. She is married, has kids, and, most important of all, is happy.
This article was previously published at Psychology Today on 5.22.2022.
Practice Aloha. Do all things with love, grace, and gratitude.
© 2022 David J. Bredehoft
References
Bredehoft, D. J., & Leach, M. K. (2006). Influence of childhood overindulgence on young adult dispositions. Executive Summary: Study 2.
Love, H., Cui, M., Hong, P., & McWey, L. M. (2020). Parent and child perceptions of indulgent parenting and female emerging adults’ depressive symptoms, Journal of Family Studies, DOI: 10.1080/13229400.2020.1794932
Centers for Disease Control and Prevention. Facts about suicide. Downloaded 04.28.22 from https://www.cdc.gov/suicide/facts/
Glasser, N. (Ed.). (1989). What are you doing? How people are helped through reality therapy. New York: Harper Colophon Books.